Abstract
Introduction: Advances in technology used to measure function and mobility may overcome barriers to their assessment in older adults with blood cancers. However, quantitative data regarding uptake and patient adherence in using such technology is mixed (Manz et al., J. Clin. Oncol, 2022), and qualitative data regarding acceptability from stakeholders is lacking. We conducted focus groups of older patients with blood cancers, their caregivers, and hematologic oncology clinicians to determine the potential benefits and barriers associated with the use of technology to measure function in the home.
Methods: We conducted three semi-structured focus groups led by a trained moderator in January 2022: two 90-minute focus groups of older patients with either myelodysplastic syndrome (MDS) or multiple myeloma and caregivers, and one 60-minute focus group of blood cancer clinicians. Eligible patients came from the Older Adult Hematologic Malignancies Program at Dana-Farber Cancer Institute (DFCI, Boston, MA), which includes adults ≥ 70 years enrolled on their initial consult visit with their oncologist. Eligible caregivers were ≥ 18 years and identified by enrolled patients as their primary caregiver. Eligible clinicians were practicing DFCI hematologic oncologists, nurse practitioners, or physician assistants with at least two years of experience. Participants were asked about their general perspectives with technology and function/mobility assessments. The study team presented examples, supplemented with brief videos, of two of the main classes of technology currently being explored for measuring function and mobility in patients’ homes: (1) intermittent wearable sensors (represented by a smartphone gait application) and (2) passive monitoring devices (represented by a contactless device that continuously measures activity). All focus groups were conducted using a secure video-conferencing platform (Zoom), recorded, and professionally transcribed. A qualitative researcher (A.C.R.) led thematic analysis, discussing each step with the interdisciplinary study team. Analysis focused on identifying key patterns, concepts, contexts, and themes within and across groups to characterize perspectives on the potential benefits and barriers associated with the use of technology to measure home functioning. This process was supported by NVivo 12 Software (QSR International, Melbourne, Australia).
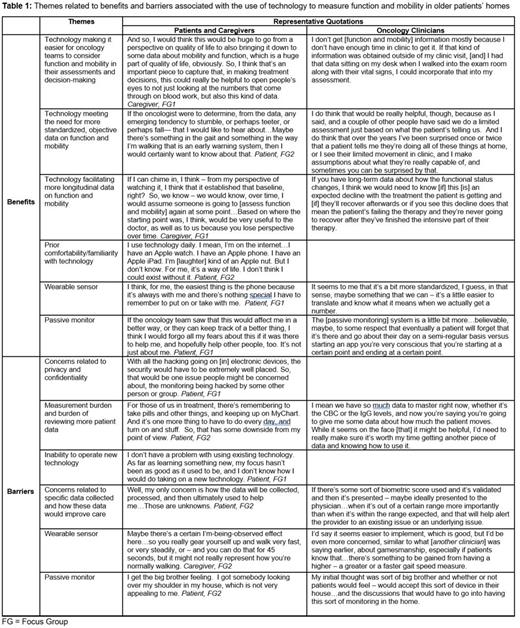
Results: Twenty-three participants attended the three focus groups: four patients with MDS, four patients with multiple myeloma, and seven caregivers attended the first two, and seven physicians and one nurse practitioner spanning specialization in leukemia/MDS (3), multiple myeloma (2), lymphoma (2), and stem cell transplant (1) attended the third. Patients, their caregivers, and oncology clinicians valued functional and mobility assessment but felt that the current approach to these assessment was insufficient. Across focus groups, we identified four themes related to potential benefits of technology that would facilitate its acceptability in measuring functioning in patients’ homes (Table 1): (1) making assessments easier; (2) providing more standardized, objective assessments; (3) allowing for more longitudinal assessments; and (4) having prior familiarity with technology in everyday life. We found four themes related to barriers of technology that may limit its acceptability in measuring functioning in patients’ homes: (1) concerns related to privacy and confidentiality; (2) burden of measurement and having to review additional patient data; (3) challenges in operating new technology; and (4) concerns related to specific data collected and how these data would improve care. The main concern specific to the wearable sensor was patients reporting they might modify their walking knowing it was being measured. The main concern specific to the passive monitor was patient privacy in having home activities continuously monitored.
Conclusion: Although patients, caregivers, and oncology clinicians reported several potential benefits of technology used to measure function and mobility in patients’ homes, they also voiced concerns about several barriers that could limit acceptability and uptake. Clinician-patient communication, best practices in data security, and further investigation will enhance implementation of these technologies in research and practice.
Disclosures
Abel:Novartis: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal